What Are the Key Methods for Immunogenicity Testing?
Immunogenicity can shape a therapy’s safety, exposure, and durability, especially for biologics such as monoclonal antibodies, fusion proteins, ADCs, cell and gene therapies. Detecting anti-drug antibodies (ADAs) early and understanding whether they bind, neutralize, or simply signal risk helps teams refine formulations, dosing, and patient monitoring. The following sections outline the core laboratory methods and validation practices that regulators expect, with practical notes on assay design, drug tolerance, and how complementary DMPK analytics strengthen interpretations.
From screening to functional impact, the immunogenicity testing methods below are typically implemented in a tiered workflow to build logical results.
Tiered ADA strategy (screen → confirm → characterize).
Most programs follow a three-step cascade. Screening casts a wide net for potential positives. Confirmatory assays verify specificity (e.g., competitive inhibition with the therapeutic). Characterization then estimates titer and explores isotype/subtype, epitope, and persistence over time. This structure balances sensitivity with specificity and ensures only true ADA signals proceed to deeper analysis and clinical interpretation.
Screening assays: bridging ECL/ELISA as workhorses.
Bridging ELISA or electrochemiluminescence (ECL) formats are widely used because they are species-agnostic and highly sensitive. The drug is labeled in two ways: ADAs, if present, “bridge” the labels to generate a signal. ECL typically offers lower background and broader dynamic range than colorimetric ELISA, supporting ultra-low detection while tolerating variable matrices common in clinical samples.
Confirmatory and characterization assays.
Specificity is usually confirmed by competitive inhibition: adding excess unlabeled drug should quench the true ADA signal. Subsequent titer and isotyping indicate magnitude and immune class, while epitope mapping and affinity (when feasible) add context to potential neutralizing risk. These data help explain exposure changes and inform risk management (e.g., premedication, route changes, or formulation adjustments).
Neutralizing antibody (NAb) assays.
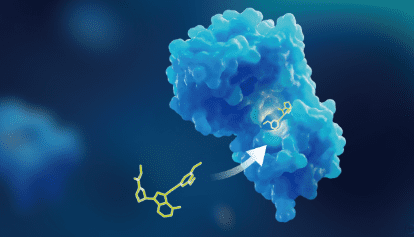
Because binding ADAs are not always neutralizing, programs include NAb tests. Cell-based assays measure loss of the drug’s biological activity in a relevant pathway and are considered most physiologically meaningful. Competitive ligand-binding NAb methods can be used when cell systems are impractical. Choice of positive control, sensitivity targets, and robust acceptance criteria is critical to avoid false negatives or overcalling.
Building drug tolerance: sample pretreatment strategies.
High circulating drug levels can mask ADAs by forming immune complexes. To restore detectability, labs use pretreatments such as acid dissociation, affinity capture extraction (ACE), SPEAD/BEAD, or PandA, which can raise drug tolerance from tens to hundreds–thousands of μg/mL. Method selection weighs sensitivity goals, throughput, and matrix complexity to minimize false negatives without inflating background.
Controls, cut-points, and validation under guidance.
Positive control antibodies (often polyclonal) establish sensitivity and drug tolerance. Programs define data-driven screening and confirmatory cut-points, MRD, precision, selectivity, specificity, hook-effect checks, robustness, stability, and reproducibility per FDA/EMA expectations; NMPA additionally emphasizes cytokine-release assessments for immune-targeting drugs. Strict QC (blanks, spikes, controls) and run acceptance rules keep longitudinal datasets comparable.
Dealing with interferences and adding orthogonal evidence.
Soluble targets can create false positives or mask ADAs; target-blocking antibodies or depletion steps improve target tolerance. Orthogonal tools enhance interpretation: SPR/BLI profile binding kinetics; LC-MS/MS tracks intact drug/metabolites; and ICP-MS/MS quantifies elemental payloads in ADCs or radiometal surrogates. In integrated DMPK workflows, these datasets connect ADA/NAb findings to shifts in exposure, distribution, and safety signals.
Conclusion
Immunogenicity testing is most effective when a sensitive screening net is paired with rigorous confirmation and clinically relevant functional assays. Strong drug-tolerance tactics, well-chosen controls, and validation aligned to regulatory guidance keep results reliable across studies. By folding in orthogonal analytics—kinetics, molecular characterization, and element-specific quantification—teams can explain why exposure changes occur and respond quickly with formulation, dosing, or monitoring strategies that protect both efficacy and patient safety.

Source: What Are the Key Methods for Immunogenicity Testing?




